- Communications
- News
- Press Release
Contact:
Bob Young
510-251-9470 |
For Release:
November 20, 2014
|
CWCI Study Monitors California Workers Comp Medical and Indemnity Trends
Payments for pharmaceuticals and durable medical equipment (DME) in California workers’ compensation continue to increase sharply, adding pressure against the recent reforms to the system according to a new CWCI study that examines medical and indemnity payment trends from accident years (AY) 2002 to 2014.
The study, based on an analysis of 2.1 million claims involving $25.6 billion in benefit payments, breaks out results by accident year, noting average amounts paid for medical services at 3 through 60 months post injury. The latest data show that while average medical payments on lost-time claims in the first two years post injury grew a modest 2.3% between AY 2011 and AY 2012, average amounts paid for pharmaceuticals and DME increased 19.4% to $2,154 -- and that came on the heels of a 26% increase in the prior year. Following legislative reforms in 2003 and 2004, pharmaceutical and DME payments declined briefly, falling in both AY 2004 and 2005, but since then they have been the fastest growing medical component in California workers’ comp, increasing more than threefold over the past 7 years. In contrast to the ongoing double-digit increases in pharmaceutical and DME payments, the 2-year data on AY 2011 and AY 2012 claims show medical treatment expenses (i.e., payments to medical providers, hospitals, outpatient facilities, and for ancillary services such as X-rays and MRIs), which accounted for two-thirds of all medical payments on those claims, and medical management/cost containment expenses (i.e., medical bill review, medical case management, utilization review and medical network fees), registered only modest increases, while payments for medical-legal reports declined.
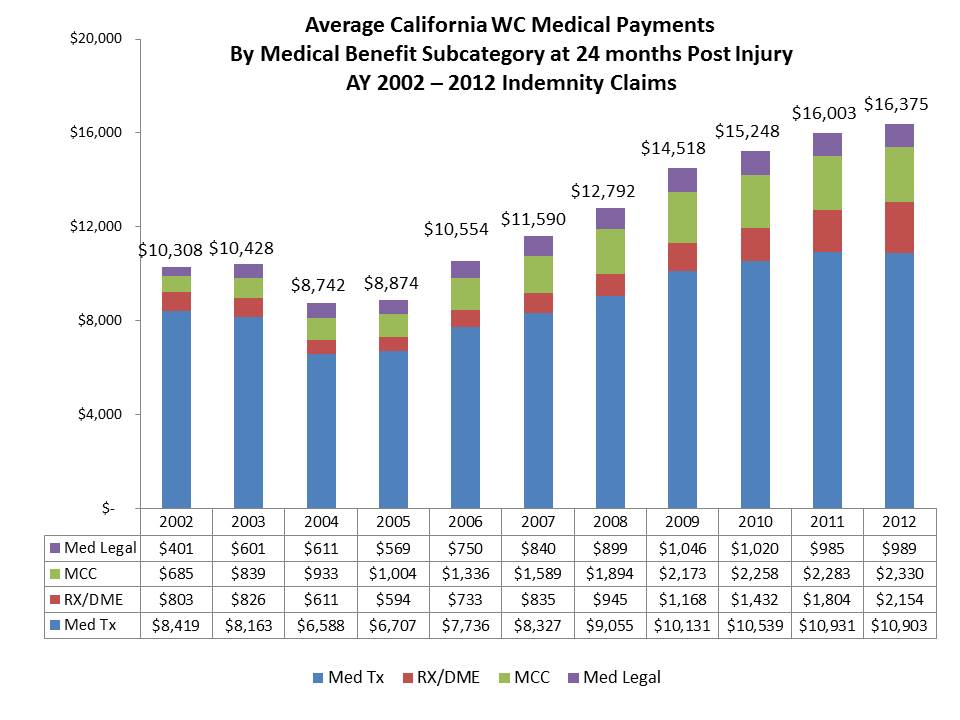
With growth rates varying among the medical subcategories over the past decade, medical treatment declined from 81.7% of all workers’ comp medical payments at 24 months in AY 2002 to 66.6% in AY 2012, while pharmaceutical/DME payments grew from 7.8% to 13.2%. Medical management payments grew from 6.6% to 14.2% over the same period, as those expenses escalated rapidly after AY 2005 as various managed care elements of the 2002-2004 reforms led to increased outlays for medical bill review, medical case management, and medical network access fees, though the 2-year data from AY 2011 and AY 2012 claims indicate they may have leveled off, albeit near record levels.
The study also offers a first view of medical experience for 2014 injury claims, showing total medical payments at 3 months post injury averaged $3,809, up 12% from $3,400 in the prior year, but such outcomes should be treated as preliminary as early treatment patterns often change due to market and regulatory factors.
In addition to identifying medical payment trends, the Institute study also provided new trend data on indemnity benefits and length of temporary disability. Among the key findings:
- At 24 months, total indemnity costs per claim for injury year 2012 were up 5.9 percent to $12,923.
- At 24 months, average temporary disability payments increased by 5.5 percent and paid temporary disability days increased by 2.9%.
The CWCI Research Update report, “California Workers’ Compensation Medical and Indemnity Benefit Trends, AY 2002–2014,” is posted on the Institute’s website, http://www.cwci.org/research.html and is available to CWCI members and Research subscribers who use their passwords to log in to the site.